Enteric tube
Enteric tube

The gastrointestinal tract is a long connection that extends from the mouth to the anus. Food travels from the mouth, to the esophagus, to the stomach, to the small intestine, to the large intestine, and finally out through the anus. The small intestine is broken down into three parts: the duodenum, jejunum, and ileum. Enteric tubes are support devices that are placed for feeding or to decompress the GI tract.
Brief description of nomenclature:
These tubes can be inserted through your nose (naso-) or mouth (oro-) and can terminate in either the stomach (-gastric), duodenum (-duodenal), or jejunum (-jejunal). The duodenal and jejunal tubes are collectively called post-pyloric tubes.
Nasogastric (NG) -
NG tubes enter the nose, run down the esophagus, and terminate in the stomach. These tubes can be placed at the bedside by your provider or someone with experience at the bedside (click link for instructions on how to place an NG tube)
Nasoduodenal (ND) -
ND tubes enter the nose, run down the esophagus, go through the stomach, and terminate in the duodenum. These are placed by a physician with x-ray guidance to ensure correct placement.
Nasojejunal (NJ) -
NJ tubes enter the nose, run down the esophagus, go through the stomach and duodenum, and terminate in the jejunum. These are placed by a physician with x-ray guidance to ensure correct placement.

Gather supplies: NG tube, dark colored marker pen, water based lubricant, adhesive skin dressing, tape, 10 mL syringe
Prepare the tube
- Wash your hands with soap and water
- One end of the tube is rounded and goes into the nose. The other end has a variable number of ports.
- The tube may have a wire inside it. This is to prevent the tube from curling while being inserted. Check that this can be removed easily.
Measure the tube
- Hold the tip of the tube at the nose, then extend the tube to the earlobe, then from the earlobe to a spot between the bottom of the breastbone (xyphoid process) and belly button.
- Keep your finger on the tube at this spot.
- Use a dark marker pen to mark this spot on the tube. This shows how much the tube needs to be inserted before it reaches the stomach.
Position the patient
- If the patient is an infant, wrap them into a blanket to prevent movement (you may need someone else to help hold your child).
- If the patient is older, have them sit upright with the chin tucked slightly toward the chest.
Insert the tube
- Apply water based lubricant to the tip of the tube so it can slide through the nose.
- Gently guide the tube into either nostril
- The tube is easier to advance when the patient is swallowing. An infant can suck on a pacifier while you insert the tube. Older patients can drink water or dry swallow. If the patient coughs, gags, or has trouble breathing, stop and wait. Allow the patient to relax then try again.
- Advance the tube until the mark you made earlier reaches the nose.
- Place adhesive skin dressing on their cheek where you plan to tape the tube to minimize skin damage. Then tape the tube in place.
- If there was a wire with the tube, remove it at this time. Don’t throw the wire away in case you need to reinsert the tube later.
- After placement of the tube, if the patient has difficulty breathing, coughing, or bluish skin or if you see the tube coiled in the back of the mouth, remove the enteric tube and start over.
Check placement of the tube
- Attach the syringe to the end of the tube and make sure the other port is closed off.
- Pull back on the plunger of the syringe to get stomach contents..
- Check the pH using pH paper. Gastric pH should be 1 to 4.
- Check the color of the fluid. Gastric fluid should be clear, light yellow, or light green.
- Disconnect the syringe.
- Make sure the tube is still in place on the patient’s cheek.
- Wash the syringe with soap and water. Wash your hands with soap and water.
Checking tube placement at home before feeding
- Gather supplies: 5 to 10 mL syringe
- Attach the syringe to the end of the tube and make sure the other port is closed off.
- Pull back on the plunger of the syringe to get stomach contents.
- Check the pH using pH paper. Gastric pH should be 1 to 4.
- Check the color of the fluid. Gastric fluid should be clear, light yellow, or light green.
- Disconnect the syringe.
- Make sure the tube is still in place on the patient’s cheek.
- Wash the syringe with soap and water. Wash your hands with soap and water.
- Proceed with feeding. Feeding instructions are described here (hyperlink here to the feeding instructions)
Flushing the tube -
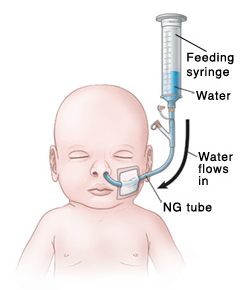
Flushing the tube for bolus feeding that is using a syringe
- Gather supplies: syringe and water
- Wash your hands with soap and water
- Attach the feeding syringe to the feeding port of the tube without the plunger. Pour water into the tube and let it run by gravity.
- If the water flows too slowly or does not flow at all, place the plunger on the syringe. Gently press the plunger to help remove anything blocking the tube. Do not push the plunger all the way in with force. Repositioning the patient so they are lying down or sitting upright can also help the flow.
- Disconnect the syringe from the tube and then close the feeding port of the tube with the cap.
- Wash your hands when you are done.
Flushing the tube for bolus feeding or continuous feeding that is using a pump
- Gather supplies: syringe and water
- Wash your hands with soap and water
- Make sure the pump is in the STOP/OFF mode.
- Make sure the clamp on the feeding bag tubing is closed.
- Disconnect the feeding bag tubing from the enteric tube
- Draw up 5 to 10 mL of water into an empty syringe. Then connect the syringe to the feeding port of the enteric tube.
- If the water flows too slowly or does not flow at all, place the plunger on the syringe. Gently press the plunger to help remove anything blocking the tube. Do not push the plunger all the way in with force. Repositioning the patient so they are lying down or sitting upright can also help the flow.
- Disconnect the syringe from the tube and then close the feeding port of the tube with the cap.
- Wash your hands when you are done.

Feeding Instructions
There are two types of feeding that can be done with an enteric tube.
Bolus feeding -
- Gather supplies: liquid food and feeding syringe
- Wash your hands with soap and water
- Check placement of the tube to confirm it is in the stomach
- Make sure the liquid food is not expired. If expired, get a new can or bag.
- Open the feeding port cap at the end of the enteric tube.
- Connect the feeding syringe to the feeding port of the tube.
- Gently pinch the enteric tube with one hand and slowly pour the food into the feeding syringe with the other hand. This keeps the food from flowing through the enteric tube until you have finished measuring it. Fill the syringe to the amount as instructed by your provider which can be found in your MDC account.
- Stop pinching the enteric tube and hold the feeding syringe straight up. This allows it to run via gravity.
- If the food flows too slowly or doesn’t flow at all, connect the plunger to the feeding syringe. Gently push the plunger to remove any blockages. Do not force the plunger all the way into the syringe.
- Refill the feeding syringe if needed to administer the total amount prescribed by your provider.
- After feeding, flush the tube with water Flushing the tube for bolus feeding that is using a syringe
- Disconnect the feeding syringe and close the feeding port on the enteric tube.
- Wash your hands with soap and water.

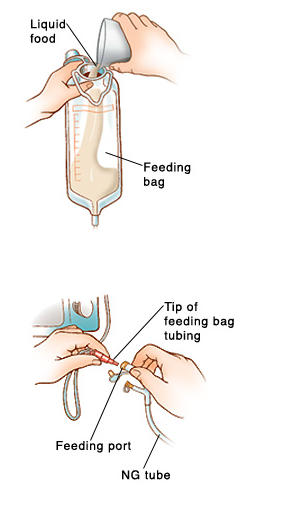
Continuous feeding
liquid food is dripped slowly through the tube via a pump
- Gather supplies: liquid food, clean feeding bag with tubing, feeding pump, syringe and water for flushing
- Check your MDC account or talk to your provider to know how much to give at each feeding and how often to feed.
- For continuous feeding, the amount of food to be given and the time frame are often set on the pump for you. Do not change the settings on the pump unless you’re told to.
- Wash your hands with soap and water.
- Make sure the pump in the STOP/OFF mode.
- Check placement of the tube to confirm it is in the stomach.Check Placement Section
- Make sure the liquid food is not expired. If expired, get a new can or bag.
- Make sure the clamp on the feeding bag tubing is closed.
- Pour a little more than the prescribed amount of liquid food into the feeding bag. Then close the top of the bag.
- Hang the feeding bag on the pole above the pump and make sure the feeding bag tubing hangs straight.
- Open the clamp on the feeding tube slowly and let a small amount of food run through the end of the feeding bag tubing. This clears air out of the feeding bag tubing which prevents the patient from having gas later.
- Load the feeding bag tubing into the pump.
- Close the clamp on the feeding bag tubing.
- Open the feeding port cap at the end of the enteric tube.
- Connect the feeding bag tubing to the feeding port of the enteric tube.
- Open the clamp of the feeding bag tubing.
- Verify the settings on the pump are correct. Then turn the pump to START/ON and let the feeding go to completion.
- After feeding, flush the enteric tube with water (click here to Flushing the tube for bolus feeding or continuous feeding that is using a pump)
- Disconnect the syringe used for flushing and close the feeding port on the enteric tube.
- Wash your hands with soap and water.

Skin Care
- Clean the skin around the tube with warm water and a wash cloth after each feeding. Remove any crusting or secretions from the nose.
- Replace the bandage or dressing around the nose every 2-3 days. Before removing the bandage or dressing, use some mineral oil or other lubricant to minimize skin irritation.
- If you notice mild irritation around the nostril, consider putting the tube in the other nostril.
Signs of infection
If you notice a fever or severe nasal redness, tenderness, warmth, a foul odor, thick yellow green drainage, call your care team immediately.
Signs that the enteric tube needs to be removed
If the patient has difficutly breathing, coughing, or bluish skin after placement of the tube. Or if you see the tube coiled in the back of the mouth.
What if I can’t pull back any stomach contents
Try to reposition the patient onto their left side and try again. If you still can’t see stomach contents, remove the tube and place a new tube. There is a chance the tube was in the lungs instead of the stomach.
How often does the enteric tube need to be changed
At least every 30 days.
Call your doctor and seek immediate medical care if you notice the following signs and symptoms:
- Signs of infection
- Increase pain, swelling, warmth, redness around drain site
- Pus draining from the insertion site
- Fever
- Sudden change in color and smell of your drainage
- Tube is coming loose out of your insertion site
